By Charley Kitely
The definition of innovation according to the Collins English dictionary is ‘something newly introduced, such as a new method or device’. But, to a cancer patient, innovation means something much more. It means opportunity, a chance and hope.
The Saatchi Medical Innovation Bill hopes to support doctors and scientists, providing them with the opportunity to question if there is a new way of managing cancer and the chance to develop treatment, perhaps even a cure. And then there is the hope doctors and scientists will refuse to accept that the standard procedure is good enough and consider a new way to treat cancer, providing people in my situation with the opportunity to test out their theory without the fear of legal recourse.
When I was diagnosed with bowel cancer in February 2012, I was asked my family history. A quick phone call to my parents revealed that unfortunately my odds weren’t great – my paternal Grandfather had died 35years previously and my maternal Grandmother some 15 years ago, both to bowel cancer.
But surely that was a long time ago and medical research has come a long way? I was only 33 when diagnosed, a young, fit and healthy mum. Surely my odds would be significantly better?
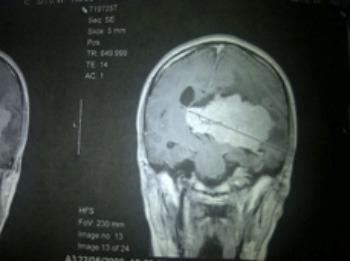
Yet 35 years after my grandfather was being treated for the same disease, we are still tackling cancer in the same way – cut, burn and poison. And whilst there has been moderate improvements on the potential side effects (for example I haven’t lost my hair, it’s just thinned and my stomach convulsions are dramatically improved with an injection prior to chemo), unless detected early, the ‘cure rates’ of bowel cancer remain disappointing.
I’m not by any means detracting from the ground-breaking work doctors and scientists are doing in the labs. There have been massive advancements in life pro-longing drugs such as Avastin and more recently Aflibercept, which have worked to keep me here, with my young family a year over my ‘expiry date’ and we are detecting cancer much earlier with better screening, though for bowel cancer patients, this is from the age of 65, not much help when you’re 33!
And this is why the Saatchi Medical Innovation Bill is so important. This bill will give doctors the opportunity to consider new drugs or techniques that could go on to save the lives of people like me. People who at the moment are written off as incurable, where the best I am offered is a comfortable quality of (shortened) life.
I am, in terms of bowel cancer patient, young and (if you forget the minor cancer detail) healthy. I lead an active life, from swimming with dolphins to teaching my 3 and 5yr olds to ski (clearly against Drs orders!), I refuse to be defined by or compromise my ambitions just because I’m fitting fortnightly chemo sessions into my life.
Given I have tried and exhausted the traditional routes, I am now looking at alternative treatment programmes to get me out of this pickle. Trials and innovation could be the answer for me surviving this disease.
We need to encourage innovation, allowing doctors a more exhaustive list of treatments to try out. I need to be able to look my doctor in the eye and ask him if he really has tried everything and if not, what else can we try.
Of course this is not to suggest my doctor will suddenly run into a laboratory, mix some random drugs together, give me an injection and hope all will be better.
R&D and drug development takes years to bring to market and for every successful drug, there are hundreds that don’t make it. And of course there are the research hospitals that already give patients the opportunity to be considered for trials.
But, this bill will make it possible for me to push for a new treatment, accepting the consequences are for me to bear. It returns some control to the patient (which is something many with cancer feel is lost when they are diagnosed) and encourages better education. Surely this can only be a good thing?
As patients, we should be open to new, exciting and alternative treatments.
There may not be the vast numbers of patients in new research, but if more of us consider new treatments rather than being scared by it, these figures will increase, prompting further confidence for other patients. We should be taking responsibility as much as the doctors in finding a cure, not only opting in to research programmes, but also taking an honest view of what we put in and around our bodies.
For me, that means avoiding things that could be considered to encourage cancer growth (sugar and dairy) and instead surround myself with things that prevent further tumours (lots of green veg and turmeric).
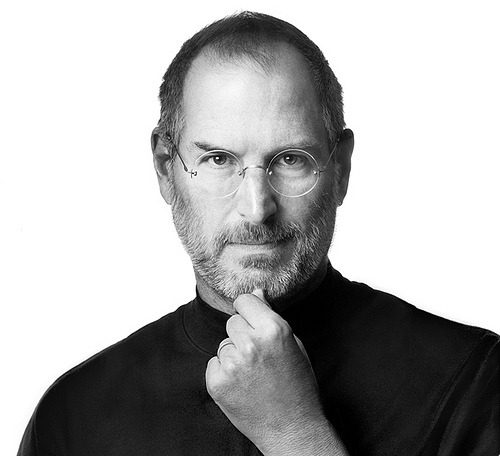
Doctors need to be encouraged to think beyond what they have always done. As Einstein once said, ‘insanity is doing the same thing over and over and expecting different results’. If we continue to treat cancer as we have for the last 40 years, we can only expect the same results – more people needlessly dying to a disease that could be curable.
Innovation has to be at the heart of the next stage of cancer research and the Saatchi Medical Innovation Bill could be the bill that makes the difference for doctors to be able to innovate and think outside the box we seem so snugly determined to remain in.